Nearly everyone has had headache pain, and most of us have had it many times. In fact, headaches and migraines affect 38 million people in the United States and is a leading cause of disability. The disease can be managed, but there is no cure, and many medications used to treat migraine have disabling side effects. Patients often prefer to avoid daily medication and seek nonpharmacologic options, including complementary and integrative therapies. Although migraine is a disease with multivariate symptoms that vary by patient, over 75% of migraine patients report associated neck pain, and many note musculoskeletal complaints, such as neck stiffness, muscle tension, or problems with jaw function. Most common triggers include:
Genetics: When studies are done on twins, there is as much as a 51 percent likelihood that they will both develop migraines. This is more likely in those with aura than those without.
Triggers: Migraines often begin with triggers. Things like food, exhaustion, and weather have been known to trigger headaches. In fact, the majority of people who have migraines report having triggers as well. The trigger can occur as many as 24 hours before the migraine hits.
Physiological characteristics: Psychological stress has been reported to be a trigger for migraines in as many as 80 percent of the cases. Other things associated with migraines are PTSD (post-traumatic stress disorder), abuse, menstruation, oral contraceptive use, pregnancy, perimenopause, and menopause.
Dietary considerations: As many as 60 percent of people say they have food triggers. Some report such things as aged cheeses, red wine, chocolate, alcohol, MSG, too much or too little caffeine, and aspartame as possible triggers. However, no substantial evidence exists to prove this.
Environmental features: Such things as changes in weather, barometric pressure, allergies, bright sunlight, lightning, and indoor air quality are potential triggers for some migraine sufferers.
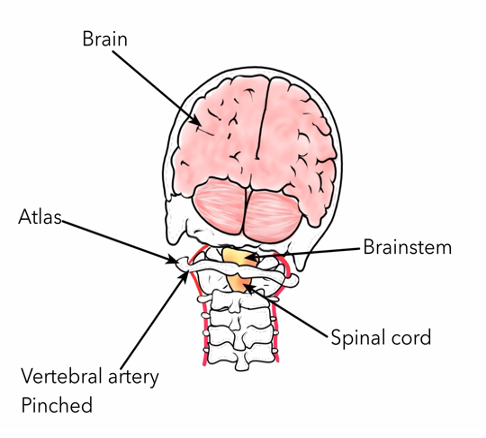
It is most likely that migraines start with a neurovascular disorder that begins in the brain and spreads to the blood vessels. The central nervous system is definitely a contributing factor, along with brainstem malfunction. Can anything be done to alleviate migraine pain? An innovative treatment using The Blair Upper Cervical Care method focuses on treating the underlying problem that causes migraines and headaches.
The missing factor: The Upper Neck
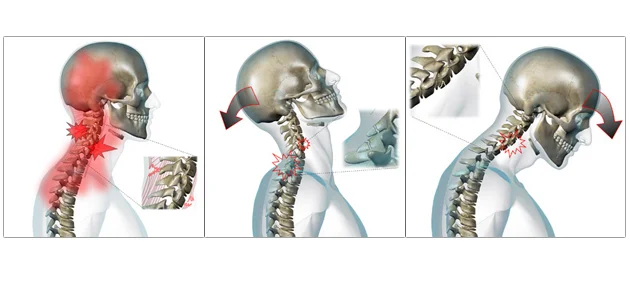
Chronic Migraine headaches are caused by many different factors. An important factor is the relationship between chronic migraine headaches and the upper neck. Specifically how the base of your skull connects to the top couple of vertebrae in the cervical spine. C1 and C2, or Atlas and Axis, as they are called, are the most freely moving vertebra in the entire spine. This gives us a great range of motion in our neck but also means that when the body has trauma, it is an area that is likely to mis-align. A misalignment at the skull base interferes with nerve pathways, blood flow, and cerebrospinal fluid flow. Compromise to any of these systems can result in the symptoms of migraine headaches. At Areté Chiropractic we are experts in evaluating the alignment of the head and neck and how that affects spinal health and body balance. If a misalignment in the C1-C2 vertebra is a contributing factor to migraine headache, then reducing or correcting that misalignment will make a significant difference in how your body functions. We can often help people's bodies function better with less symptoms, or even recover completely.
A Study Gives Hope for Migraine Relief
In 2012, the Journal of Chiropractic Medicine relayed the findings of a study that involved a woman suffering from migraines and tremors. They were observing how the Blair technique, a specific type of upper cervical adjustment given by upper cervical chiropractors, would impact her health.
The woman was 39 years old and was having a migraine as many as 2 or 3 times a week. She had a history of having migraines since she was 10 years old. Her family doctor prescribed various medications — acetaminophen, sumatriptan, Isometheptene, dichloralphenazone, propranolol, and numerous other over-the-counter pain medications — to no avail. While they gave her some relief, it was only temporary at best.
She agreed to give upper cervical chiropractic care a try. She received specific adjustments to her upper cervical spine, specifically the C1 (atlas) and C2 (axis) bones of the upper neck. After her very first adjustment, she noticed that her migraines and tremors were both improved! She continued seeing good results over the next four months.
The headache disability scale was used in her evaluation. This is a scale using 1 – 100 points (52 for emotional and 48 for functional disability) to indicate how much damage the headache being endured is causing in one’s life. The higher the score, the greater the disability. These were her results before having her adjustment by the chiropractor:
Total: 68/100
Emotional: 28/52
Functional: 32/48
After four months of care, she was re-evaluated and these were her new scores:
Total: 14/100
Emotional: 4/52
Functional: 10/48
This is truly good news if you suffer from migraines!
What is Upper Cervical Chiropractic Care?
Upper Cervical Chiropractic spinal corrections provide relief to millions of migraine sufferers by releasing pressure and stress from the spine and nervous system. Research from 2015 showed that people who received upper cervical manual adjustments reduced their drug consumption by 80%, lowered days of migraines per month by 97%, and experienced an amazing decrease in pain and functional disability associated with migraines by 100%.
Nutrition, stress, hormones, and other lifestyle factors also play a role in the intensity and extent of migraines. The core of all of these factors connects to the role of the central nervous system. The brain and nervous system direct the control and function of the entire body. Chiropractors assess and address specific areas of function in the nervous system through appropriate care of the spine. Every Upper Cervical Chiropractic adjustment helps improve communication between the brain and the body, reducing stress from the central nervous system.
Five lifestyle tips to address the cause of migraine headaches:
1) Chiropractic adjustments to correct spinal alignment and pressure in the upper neck
2) Remove dietary neurotoxins (artificial colors, sweeteners, and preservatives)
3) Increase water intake
4) Increase high quality sleep
5) Engage in regular body movement through exercise and increased heart rate
WHY MEDICATION IS OFTEN INEFFECTIVE FOR CHRONIC MIGRAINES
While medication may temporarily help with the symptoms of a migraine, there is no miracle pill that will stop the next migraine from occurring. Plus, many medications can produce more headaches when taken frequently and for long periods of time. The result is a cycle where one medication is taken to deal with migraine headache pain until it begins causing them and then the medication is switched, and the process starts again.
Other treatments involve dangerous Botox injections or a journal in which you record foods, activities, etc. to determine potential migraine triggers and avoid them. Are you tired of the run-around, the trial and error, and the side effects?
UPPER CERVICAL CARE FOR MIGRAINES
Using the Blair technique, we locate and correct very specific misalignments of the upper neck. Such misalignments can result in reduced blood and cerebrospinal fluid flow to the brain. They can also affect communication in the body by placing pressure on the brainstem, as well as creating muscle tension and joint dysfunction. Once these issues are relieved through an adjustment, healing can begin.
So, if you or someone you know suffers from migraines, Upper Cervical Chiropractic care may be a very helpful tool to regain quality of life and function. Call our office today to find out more or to schedule an Initial Consultation today.